
Pharmaceuticals Alone Are Not The Answer To Achieve Long-Term Recovery From Opioid Addiction
It is a uniquely American way of thinking that a pill can fix us. According to Consumer Reports, “The total number of prescriptions filled by all Americans, including adults and children, has increased by 85% over two decades, while the total U.S. population has increased by only 21%.” between 1997-2016 and this has only gotten worse over the last 5 years.
According to Harvard research in 2019, “The opioid crisis is not a global phenomenon but a uniquely American one – our residents use an estimated 30 times more opioids than is medically necessary, and we consume 99% of all hydrocodone in the world.” And according to the CDC in December of 2020 , “Over 81,000 drug overdose deaths occurred in the United States in the 12 months ending in May 2020, the highest number of overdose deaths ever recorded in a 12-month period”.
There are four main drugs used for MAT (medically assisted treatment), the “gold standard” by the NIH (National Institute of Health) for treating opioid addiction. When properly dosed and managed, MAT can prevent opioid withdrawal, reduce cravings, and block or lessen the euphoric effects of other opioids such as heroin/fentanyl/Oxycodone. The first three are used in detox and ongoing treatment and the fourth is primarily used as a means of reversing opioid overdoses:
- Buprenorphine - sold alone as Subutex and with Naloxone as Suboxone, both typically prescribed as daily prescriptions. Buprenorphine is a partial agonist, meaning it only partially activates opiate receptors compared to full fast acting full agonists like heroin/fentanyl/Oxycodone. Naloxone is an opioid antagonist so it blocks opioids at the receptor sites. Together they have less of an opportunity for abuse. Longer acting implants are also available, but are costly and less popular, and have an addiction potential.
- Naltrexone - sold as a daily prescription or as a long acting monthly shot called Vivitrol. Longer acting implants are also available, but are costly. As stated above it is an opioid antagonist, so you can’t begin taking it until after you have gone through detoxification of up to two weeks from opioids or it will cause severe withdrawal symptoms, so alone it is less popular. This has no addiction potential.
- Methadone – usually comes in a liquid administered daily in a medically supervised clinic, and is a full agonist opioid that has a lower peak high and releases over a longer period of time than other fast acting opioids like heroin/fentanyl/Oxycodone. This has no addiction potential.
- Naloxone – sold as Narcan as an injection/auto-injection or nasal spray designed to reverse opioid overdose. As described above it is an opioid antagonist, that can block the effects of other opioids. It can very quickly restore respiration to a person whose breathing has slowed or stopped as a result of overdosing with heroin or prescription opioid pain medications. This has no addiction potential.
Various studies, including systematic reviews of the research, have found that MAT can cut the all-cause mortality of opioid SUD (substance use disorder) by half or more. So, it’s not surprising that various public health groups such as the CDC, NIDA (the National Institute on Drug Abuse), and the WHO recommend it. There has also consequently been a passionate and escalating public outcry by family and friends who have lost loved ones to opioid overdoses for more access to these treatments, education, and less stigma, so others don’t have to go through the grief that they are left to endure. There are some disadvantages to using Buprenorphine based MAT which should be considered, such as:
- Maintaining dependence
- Allowing for drug diversion
- Withdrawal can take 3-4 weeks and be difficult
- It generally requires daily or multiple daily doses, which can be expensive.
Aside from these commonly discussed disadvantages, the following are some additional significant areas of concern about MAT as a long-term solution to opioid addiction recovery:
- Misuse and abuse of MAT:
-
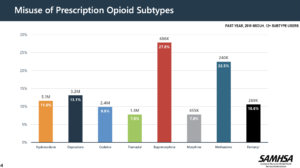
- According to the 2019 NSDUH report (National Survey on Drug Use and Health, pg. 14) Buprenorphine and Methadone remain the most misused prescription opioids in the U.S.
-
- Another NIH study concluded that “Overall, buprenorphine diversion and misuse appear to be common behaviors of opioid addicted individuals”.
-
- Even Naloxone has some controversial health policy aspects to its use as it relates to the lack of a significant decrease in overdose deaths. This study on the Systematic Evaluation of State Policy Interventions Targeting the US Opioid Epidemic, 2007-2018 states, “Naloxone laws provide civil immunity to licensed health care professionals or lay responders for opioid antagonist administration. Although expanded access to naloxone can reverse an opioid overdose and save lives, we found that naloxone access laws were associated with a substantial increase rather than a decrease in overdose deaths, especially deaths from illicit drugs. It is possible that the prospect of getting access to overdose-reversing treatment may instead induce moral hazards by encouraging people to use opioids and other drugs in riskier ways than they would have without the safety net of naloxone.”
- Non-compliance and Relapse Rates with MAT:
-
- Non-compliance rates are high with any prescribed medication having to be taken routinely over a long period of time. The New England Journal of Medicine states, “Poor adherence to medication regimens is common, contributing to substantial worsening of disease, death, and increased health care costs.”
-
- For the average person in the U.S., adhering to a medical regimen is tough (according to a 2011 study up to 75 percent don’t adhere to daily dose prescriptions). For someone in the grip of addiction, it’s near impossible.
-
- In 2011, the first large and randomized multi-site trial of patients dependent on prescription opioids showed 92% relapsed to opioids after a 12-week MAT Suboxone treatment. Additionally, only 7.2% of patients receiving counseling with the treatment and 6.2% of patients receiving the MAT treatment without counseling stayed abstinent from opiates (other than the MAT) during the full trial. There are similar high relapses after cessation rates for Methadone as well.
- There is no MAT for Poly-substance Addiction:
- There are increasingly more people seeking recovery that have poly-substance use disorders combining opioids and stimulants (cocaine and methamphetamine) where MAT is less effective since there isn’t currently an effective MAT for stimulants.
- A research study from 2018 in The American Journal of Drug And Alcohol Abuse showed bup-nx (Suboxone, a combination of buprenorphine and naloxone) and 70-83% of those prescribed Suboxone by a physician took other drugs or alcohol to get high while taking it and 80-84% sold, traded, or gave away some of the Suboxone they were prescribed. Additionally, it states in its discussion “This study suggests an emerging population of individuals with bup-nx use who are decidedly polysubstance users with extensive drug use histories – not just a clear opioid dependence pattern. Consistent with this pat- tern, more of the Recent Bup-nx Users reported taking other drugs even while on bup-nx in order to get high.”
- Another poly-substance opioid and methamphetamine study in 2018 alarmingly states, “From 2011 to 2017, methamphetamine use nearly doubled from 18.8% in 2011 to 34.2% of all opioid users in 2017 entering a drug treatment program. Of note, among those using both methamphetamine and opioids, such use was not separated but often linked together, with the majority using both drugs within the same day, and even more concerning, doing so for nearly half the days of an average month.”
Nationally recognized interventionist Earl Hightower said in remarks at the 2014 National Rx Drug Abuse Summit on Medication Assisted Treatment for Opiate Addiction, “Hear me clearly, addiction has major neurological aspects, which for some people may be chronic or lifelong in duration. The more severe the brain dysfunction and the more protracted the course of recovery, the more likely it is the individual will need medications to achieve sustained sobriety. I’m not against MAT…In fact, probably the best course of treatment for an opioid dependent person is to use medications, including buprenorphine to detox the individual and once fully detoxed, place them on Vivitrol, the long-acting, injectable naltrexone. Once stable, immerse them in a year or more of intensive psychosocial counseling, trauma and other mental health therapy, 12-step work, and close monitoring.”I wholeheartedly agree that a holistic approach to recovery over a year plus period of time incorporating the elements that Earl Hightower mentions above provides the best long-term outcomes eventually through abstinence based recovery.It would be revolutionary if taking a pill could cure opioid addiction or any other SUD, but that just isn’t the case. As it says in the AA Big Book (the origin of all 12 step groups), “Physicians who are familiar with alcoholism agree there is no such thing as making a normal drinker out of an alcoholic. Science may one day accomplish this, but it hasn’t done so yet.” And even with the tremendous scientific and pharmaceutical advancements that have been made in the last 70+ years since the book Alcoholics Anonymous was written, this remains true today for both alcoholism and opioid addiction. Over the last 33 years of my work with those seeking recovery from opioid addiction and other substance use disorders demonstrates they will either seek relief in their recovery or in their active addiction. Regardless of those seeking recovery’s life experiences, they discover their active addiction provides a short-term fix for long-term existential maladies like self-loathing, apathy, broken relationships, lack of motivation and isolation, which is why while seeking recovery it is so crucial that you find a sense of connection and community with your sober support group. If those seeking recovery aren’t willing to put as much effort into their recovery in all areas of their life (mind, body and spirit) as they did to pursue their active addiction they will find no lasting recovery.
